I had the opportunity to present Insights into “Black and Hispanic Medicaid recipients’s experiences with the healthcare system that can be used to inform the delivery of culturally tailored services: an online patient panel survey,” at the Centers for Medicare & Medicaid Services (CMS) 2024 Health Equity Conference.
Value Based Care (VBC) is center stage as the future of healthcare in the U.S. In fact, actuary experts estimate that VBC is growing at an accelerated rate, with the projected growth in VBC from $500 billion to a potential $1 trillion.
HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores impact VBC reimbursement. CMS requires that health systems administrators collect HCAHPS surveys on the patient experience. In 29 questions, the survey assesses patients’ perceptions about their care, including communication with nurses and doctors, staff responsiveness, cleanliness and quietness, and discharge process.
If VBC is the future US healthcare landscape, then patient experience is the “holy grail” for both patients and providers. For patients, research has shown that better patient experiences are associated with less healthcare utilization and better adherence to recommended prevention and treatment, clinical outcomes, and patient safety within hospitals. For hospitals, physician groups, and other healthcare providers, better patient experiences are a business imperative to achieve higher reimbursement, larger margins, and operational efficiency and cost reduction. For example, patients taking HCAHPS are asked to answer what’s called the Net Promoter Score question: Would you recommend this hospital? This is an important healthcare business metric, as it predicts the likelihood of both reengagement with a healthcare system or provider and referral which can, in turn, impacts revenue in a VBC environment.
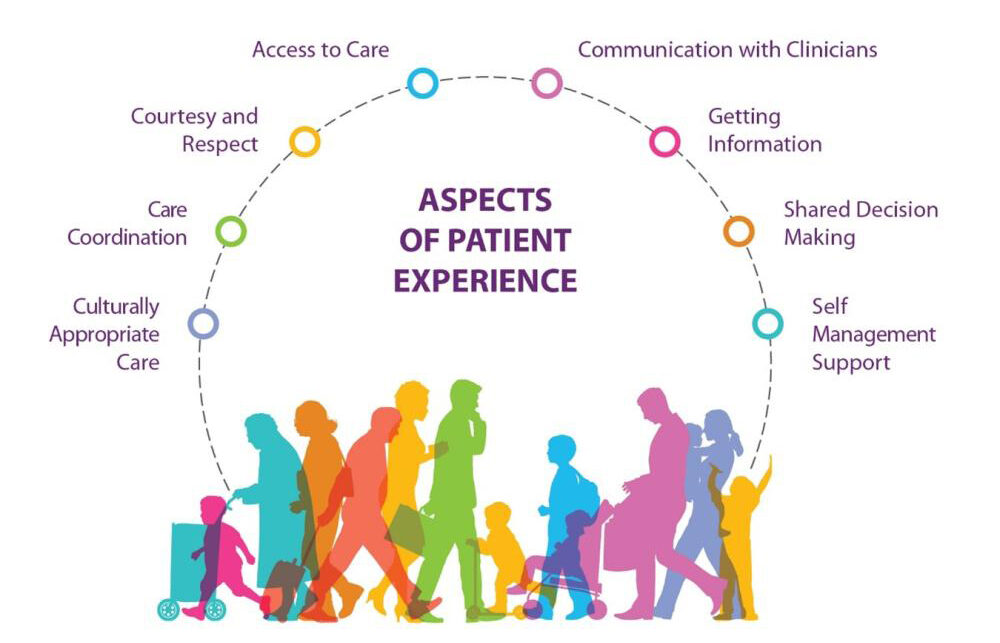
What if healthcare systems and providers are missing key insights and measures related to the patient experience? Increasingly, research is pointing to racial/ethnic discrimination and trust as overlooked and understudied indicators of patient experience and drivers of health disparities. The Agency for Healthcare Research Quality (AHRQ) defines patient experience as eight domains that include “the range of interactions that patients have with the healthcare system, including their care from health plans, and from doctors, nurses, and staff in hospitals, physician practices, and other healthcare facilities. As an integral component of healthcare quality, patient experience includes several aspects of healthcare delivery that patients value highly when they seek and receive care, such as getting timely appointments, easy access to information, and good communication with health care providers.”
However, our current measures of patient experience in the US do not include measures of racial-ethnic discrimination or trust. These oversights are bad for patients and businesses, as it’s impossible to take corrective action and do better if problems aren’t identified through robust data collection and analysis.
My presentation renders notable findings that value adds to the field of measuring patient experience and perhaps modernizing patient experience measures (M-PEMs). M-PEMs refer to applying a health equity lens to patient experience data collection and analysis plus elevating patient experience measures to include focuses on racism and trust.
Let’s face it, post-COVID-19, health equity appropriately monopolizes healthcare conversations. However, we have obfuscated racism and trust as drivers of health inequities. We need to examine racism and trust (or lack thereof) as drivers of health inequities. In practice, this means modernized patient experience measures would examine racial/ethnic discrimination and trust as additional indicators of the patient experience.
This data and call to action for the collection of patient experience data on racial ethnic discrimination and trust is in lock step with CMS commitment to data transparency, as evidenced by the release of several demographic data enhancement reports in 2023. As the AHRQ notes, “Understanding patient experience is a key step in moving toward patient-centered care. By looking at various aspects of patient experience, one can assess the extent to which patients are receiving care that is respectful of, and responsive to, individual patient preferences, needs, and values.”
The online survey and report were part of a 2023 collaboration between Atlantic Insights, the marketing research division of The Atlantic, on a global study aimed at uncovering healthcare gaps and helping leaders prioritize steps to address them, reviewed by OPRG and its key stakeholder networks, and executed by Lucid, a subsidiary of Cint.
The survey included 35 questions, fielded to 6,001 total respondents across four countries: the United States, United Kingdom, Germany, and Spain (1,500n for each country). The margin of error is 5% at the 95% confidence level. No weighting was applied to the survey. Survey was fielded March 9-24, 2023. Margin of error across the full study is +/- 5p (95% confidence), while each geo’s MoE is +/-10p (90% confidence). The differences across cohorts highlighted specifically in the country-by-country insights in the report are statistically significant at the 90% confidence level.